Introduction
True self-directed weaning rarely occurs before a child’s first birthday. Most children continue breastfeeding until at least 18 to 24 months unless actively guided toward weaning by their mothers.
Despite this pattern, many parents report their infants “naturally stopped breastfeeding” as early as 9 or 10 months old. These accounts appear contradictory—how can such experiences align with broader observations of infant feeding behavior?
This discrepancy raises important questions. Are these cases truly examples of independent weaning, or might other factors influence the perception of early self-weaning? Exploring this tension offers insight into infant development and parental interpretation of feeding transitions.
Understanding Self-Weaning in Children
A child naturally transitioning away from breastfeeding typically exhibits specific developmental markers. Such children are usually at least one year old, with many continuing to nurse until age two or beyond. By this stage, solid foods form the primary source of their nutritional intake, and they demonstrate consistent ability to drink independently from a cup. The weaning process occurs gradually, marked by a steady reduction in breastfeeding sessions over time.
True child-led weaning reflects a child’s diminished need for nursing—both for nourishment and emotional comfort. This process inherently excludes infants under 12 months, as breast milk remains critical for their optimal physical growth and cognitive development during the first year. Before this age, sustained reliance on breastfeeding is biologically essential, making genuine self-weaning improbable in younger babies.
Perceived Early Self-Weaning: Common Influences
When a mother believes her infant has self-weaned before age one, this perception often stems from misinterpretations of natural developmental shifts, sometimes intertwined with her own expectations. Reduced milk supply may further contribute to the assumption of intentional weaning.
A decline in milk production can diminish a baby’s enthusiasm for nursing, creating a cycle where less frequent breastfeeding further reduces supply. Infants may begin favoring cups or bottles if they yield more milk efficiently. Sustained milk production relies on responsive breastfeeding—allowing the child to nurse freely and drain the breasts ensures supply aligns with demand. However, several factors after lactation establishment can disrupt this balance, particularly during the latter half of the first year:
Infrequent nursing sessions due to rigid feeding schedules, excessive pacifier use, or sleep training may suppress milk supply. The threshold for “too little” nursing varies between mother-child pairs, but a sustained drop in breastfeeding frequency signals the body to reduce milk synthesis.
Sudden maternal weight loss from severe calorie restriction can impair milk production. Similarly, certain medications or herbs, such as hormonal contraceptives, may inadvertently lower supply.
Introducing solid foods before six months not only compromises immune development but often displaces breast milk intake, diminishing supply. Even after six months, abruptly increasing solid food quantities risks displacing essential milk consumption. While a gradual decline in milk supply is expected as solids become a dietary staple, maintaining breast milk as the primary nutrition source remains critical for growth and neurological health throughout infancy.
For strategies to address low milk supply, refer to dedicated resources on enhancing lactation.
Understanding Shifts in Infant Feeding Patterns
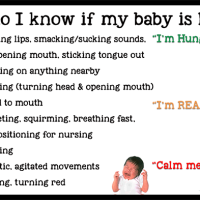
It is natural for infants to exhibit reduced enthusiasm for breastfeeding during their second half-year of life. This behavioral shift reflects typical developmental progress rather than a deliberate intention to stop nursing.
As babies grow older, they often become easily distracted, prioritizing exploration of their surroundings over daytime feeding. Many compensate by increasing nighttime nursing to fulfill nutritional needs. The convenience of bottles or sippy cups—allowing mobility while drinking—may further divert attention from breastfeeding, which requires temporary stillness. This contrast can lead some infants to favor containers during this phase of heightened curiosity.
Developmental leaps like crawling, walking, or teething, alongside stressors such as illness, frequently disrupt nursing routines. Temporary breastfeeding strikes (sudden refusal to nurse) also peak around this age, likely influenced by these overlapping factors.
Societal pressures emphasizing early independence—through milestones like solo sleep, nighttime weaning, or potty training—often overshadow biological readiness. Many caregivers misinterpret temporary disinterest as permanent readiness to wean, overlooking the possibility of resuming breastfeeding after transitional periods.
While maternal decisions to wean during this stage remain valid personal choices, it is crucial to distinguish between temporary developmental phases and true self-weaning. Mothers leveraging this window for intentional weaning should recognize it as a caregiver-guided transition rather than infant-led cessation. Awareness of this distinction empowers informed decisions about whether to continue nurturing through breastfeeding or adapt to evolving family dynamics.
Sustaining Breastfeeding Through Developmental Shifts
To prevent premature weaning, prioritize breast milk as the cornerstone of your child’s nutrition during their first year. If concerns about low milk supply arise, proactively address them through lactation support. Introduce solid foods cautiously, ensuring breast milk remains the primary dietary focus. A gradual transition—such as 25% solids at 12 months, scaling to 80% by 24 months—helps maintain milk production while meeting evolving nutritional needs. Limit sugary drinks and excessive water intake, as these can suppress hunger cues critical for breastfeeding.
Minimize reliance on bottles or cups by reserving them for unavoidable separations. Opt for slow-flow nipples or transition to cups after six months to avoid flow preferences. Reduce pacifier use in your presence, allowing natural sucking instincts to reinforce breastfeeding. Discourage mobile drinking habits—such as carrying sippy cups while exploring—to preserve the nurturing connection of nursing sessions.
For distractible infants, experiment with creative nursing positions that accommodate curiosity, such as sitting face-to-face or standing supported. Engage their attention through songs, stories, or tactile toys during feeds. A colorful nursing necklace or scarf can serve as a gentle focal point.
Examine personal habits that unintentionally encourage weaning. Offer the breast proactively rather than waiting for requests, and honor delayed nursing promises consistently. Avoid restrictive routines like scheduled feeds or designated nursing areas, which signal weaning. Nighttime nursing, especially in shared sleeping spaces, often sustains milk supply while supporting parental rest. If reducing night feeds becomes necessary, compensate by increasing daytime nursing opportunities.
Maintain physical closeness through frequent carrying and holding, reinforcing easy access to breastfeeding. Recognize developmental phases—such as teething or mobility milestones—that temporarily reduce nursing interest. By aligning with these natural rhythms rather than misinterpreting them as readiness to wean, caregivers can make informed choices that balance family needs with the biological benefits of extended breastfeeding.