Are you planning for a second child while continuing to breastfeed your firstborn? Or perhaps nurturing your little one as your growing baby bump reminds you of the new life within? You’re not alone. Research involving 179 mothers who breastfed for at least six months revealed that 61% continued nursing during a subsequent pregnancy. Among them, 38% later nursed both their newborn and older child simultaneously—a practice termed “tandem nursing”.
Maintaining breastfeeding can offer significant benefits. Human milk provides ongoing nutritional and immune support for as long as a child nurses. Studies indicate that weaning before age two may increase a child’s susceptibility to illness. The American Academy of Pediatrics recommends breastfeeding for at least one year, while the World Health Organization advocates for two years or longer. Beyond health benefits, continued breastfeeding may ease a toddler’s transition to siblinghood. It also offers a practical way for expectant mothers to rest while caring for an active child.
However, balancing breastfeeding with pregnancy requires careful consideration. Factors such as maternal rest, adequate weight gain, and overall well-being are crucial. Many mothers experience discomfort or agitation during pregnancy-related nursing, which may prompt weaning. Milk supply often diminishes by mid-pregnancy, leading some children to self-wean, while others adapt to the changes.
A common concern is whether breastfeeding-induced uterine contractions could trigger preterm labor or miscarriage. While breastfeeding stimulates oxytocin release, which causes mild contractions, these are typically harmless in uncomplicated pregnancies. However, rare cases of placental abruption linked to breastfeeding have been reported, emphasizing the need for individualized medical guidance.
To address these questions comprehensively, extensive research and interviews with over 200 mothers were conducted. The findings, detailed in the book Adventures in Tandem Nursing: Breastfeeding during Pregnancy and Beyond (La Leche League International, 2003), aim to empower parents with evidence-based insights for informed decision-making.
Breastfeeding and Uterine Contractions
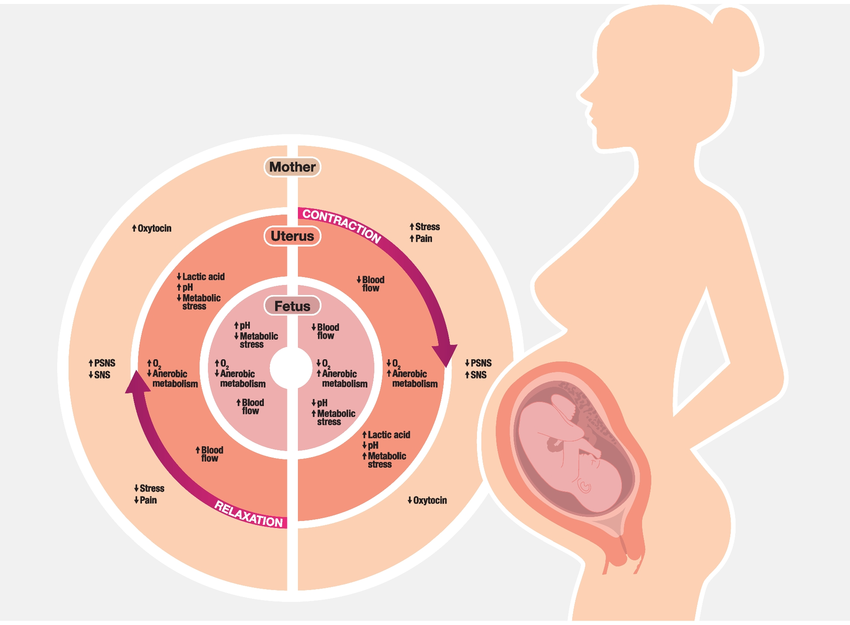
Nipple stimulation during breastfeeding triggers the release of oxytocin, a hormone critical for lactation and uterine function. Oxytocin’s dual role includes prompting breast tissue contractions to facilitate milk ejection (the “let-down reflex”)and stimulating uterine contractions. While all breastfeeding mothers experience uterine muscle activity, these contractions are typically subtle and go unnoticed. Clinically, nipple stimulation is sometimes used to aid cervical ripening during full-term pregnancies and to enhance labor progression. Postpartum breastfeeding further accelerates uterine involution, helping the uterus return to its pre-pregnancy size.
A common concern is whether breastfeeding might induce preterm labor. Although limited formal studies exist, preliminary evidence suggests compatibility between breastfeeding and healthy term pregnancies. For example, a 1993 survey of 57 Californian mothers who breastfed during pregnancy found no adverse effects on gestation. Anecdotal reports also support this, with many mothers successfully nursing throughout pregnancy and delivering healthy babies. However, breastfeeding does not eliminate risks inherent to pregnancy, such as miscarriage or preterm labor, which occur independently of lactation.
Notably, 93% of participants in the aforementioned survey reported no noticeable contractions while breastfeeding during pregnancy. Even when intense “nursing contractions” occur, they often subside shortly after breastfeeding ends. Similar to Braxton-Hicks contractions, these episodes typically do not threaten pregnancy stability. The underlying mechanisms remain an area of scientific interest, highlighting oxytocin’s complex interplay in both lactation and uterine physiology.
Revisiting the Physiology of Uterine Protection During Pregnancy
The concern that breastfeeding might induce preterm labor often stems from an oversimplified understanding of oxytocin’s role and uterine responsiveness during pregnancy. Notably, nipple stimulation releases less oxytocin in pregnant individuals compared to non-pregnant states. This hormonal dynamic is critical to interpreting the interplay between breastfeeding and uterine activity.
Central to this discussion is the uterus itself. Contrary to common assumptions, the uterus remains largely unresponsive to oxytocin throughout the 38-week preterm period. Even high doses of synthetic oxytocin (e.g., Pitocin) rarely initiate labor before term. This resilience arises from the uterus existing in two distinct states: a **”quiescent” phase** for sustaining pregnancy and an **”active” phase** for labor. During the quiescent phase, the uterus is physiologically “muffled” to oxytocin’s effects, ensuring stability until term.
Key protective mechanisms include:
- Oxytocin Receptor Density: Receptor sites on uterine cells remain sparse until 38 weeks, increasing gradually post-term and surging 300-fold after labor begins.
- Gap Junction Proteins: These proteins amplify oxytocin’s effect on receptors. Their absence during pregnancy keeps the uterus “down-regulated,” limiting responsiveness even if receptor numbers rise.
- Progesterone’s Role: This hormone acts as a natural oxytocin antagonist, blocking receptor activation and maintaining uterine quiescence.
Together, these factors create a robust defense system, safeguarding against preterm labor triggered by oxytocin fluctuations.
Balancing Breastfeeding and Pregnancy Safety
While definitive research on breastfeeding’s role in preterm labor remains limited, existing evidence suggests compatibility with healthy pregnancies. For instance, respected sources like the American Academy of Family Physicians and experts such as Dr. Ruth Lawrence affirm breastfeeding’s safety in uncomplicated pregnancies. Even in high-risk scenarios, many mothers successfully breastfeed while managing conditions like threatened preterm labor.
Clinical guidance emphasizes individualized care. Caregivers may monitor uterine contractions, fetal heart rate, or cervical changes during breastfeeding sessions. If concerning contractions arise, pausing breastfeeding and assessing their resolution—similar to Braxton-Hicks contractions—is advised.
Practical Recommendations for Concerned Mothers
- Monitor Contractions: End breastfeeding sessions if contractions persist or intensify, then hydrate, rest, and lie on your left side.
- Seek Immediate Care if experiencing ≥4 contractions/hour, pelvic pressure, or fluid leakage.
- Collaborate with Providers: Develop a tailored plan integrating breastfeeding goals and pregnancy health.
A Personal Reflection
During my second pregnancy, breastfeeding my toddler initially sparked fears of complications. Supported by midwives experienced in tandem nursing, I continued breastfeeding and later welcomed a healthy term baby. Witnessing my children nurse together underscored the body’s remarkable capacity to nurture life—a testament to the resilience of the “quiescent” uterus.
Ultimately, each mother must weigh her unique circumstances, guided by medical insight and bodily cues. Trust in your ability to navigate this balance.