Breastfeeding and Fertility: Understanding Postpartum Contraception
How does breastfeeding help prevent pregnancy?
The Lactational Amenorrhea Method (LAM) is a natural contraceptive approach that leverages the temporary infertility linked to breastfeeding. This method relies on hormonal changes during lactation, which suppress ovulation and menstruation. However, conflicting advice about its reliability often creates confusion.
Common Misconceptions
One widespread myth is that breastfeeding cannot reliably prevent pregnancy. Another is that any breastfeeding—regardless of frequency or the return of menstruation—automatically ensures contraception. Both assumptions are inaccurate.
Conditions for Effectiveness
Research shows that exclusive breastfeeding can be 98–99.5% effective as contraception, but only when strict criteria are met:
- The infant must be under six months old.
- The mother’s menstrual cycles must not have resumed.
- Breastfeeding must be frequent (day and night, without long intervals) and exclusive—meaning the infant receives no formula or solid food, except minimal complementary items.
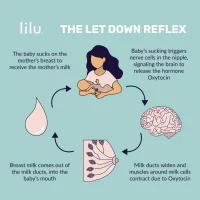
This method works by maintaining elevated prolactin levels, which inhibit ovulation. Deviations from these conditions, such as introducing formula or extended gaps between feeds, significantly reduce its effectiveness.
Extending Postpartum Infertility Through Breastfeeding Patterns
How can nursing mothers naturally prolong their temporary infertility phase?
The duration of postpartum infertility varies significantly among women and depends on both infant feeding behaviors and maternal hormonal sensitivity during lactation. Research indicates that breastfeeding frequency and total daily nursing time strongly influence fertility restoration. Reducing nursing sessions abruptly—especially cutting nighttime feeds—may accelerate fertility return, while consistent breastfeeding (including night nursing) tends to delay ovulation. Studies show mothers separated from infants but pumping milk exclusively face higher pregnancy risks (5.2%) within six months compared to those practicing direct breastfeeding.
Introducing solid foods may affect fertility restoration, but mothers can mitigate this by gradually offering solids after breastfeeding sessions and maintaining unrestricted nursing. A method called ecological breastfeeding optimizes natural infertility through specific practices:
- Maintaining constant physical proximity to the infant
- Feeding on demand (day and night)
- Using breastfeeding for comfort
- Nursing in reclined positions during naps and nighttime
- Avoiding artificial nipples like bottles or pacifiers
Data from ecological breastfeeding practices reveal pregnancy risks remain near zero in the first three months, below 2% between 3–6 months, and approximately 6% after six months (if menstruation remains absent). On average, menstrual cycles resume around 14.6 months for mothers following this approach. Early cycle resumption often involves initial infertile cycles, while late resumption increases the likelihood of ovulation preceding the first period.
Though rare, pregnancy can occur before the first postpartum menstrual cycle (the “warning period”). Most mothers only regain fertility after menstruation resumes, with some requiring multiple cycles to conceive and others needing full weaning. These patterns highlight how breastfeeding behaviors shape hormonal responses and reproductive recovery.
Phases of Postpartum Fertility Recovery
The restoration of full reproductive capacity follows a gradual biological progression. Research highlights that ovarian activity resumes incrementally, with distinct physiological milestones preceding complete fertility restoration.
Initial follicular activity may occur without ovulation, presenting no pregnancy risk. Some women experience menstrual bleeding during this phase without actual ovulation, though this pattern isn’t universal. The subsequent stage involves ovulation with inadequate luteal support: while an egg may be released and fertilized, insufficient preparation of the uterine lining often prevents successful implantation. Full fertility is only restored when the luteal phase achieves full competence, at which point breastfeeding no longer influences pregnancy likelihood.
Menstrual cycles without ovulation are most frequent within the first six months postpartum. For some, menstruation resumes before ovulation, while others ovulate before their first postpartum period—a likelihood that increases with prolonged lactational amenorrhea. Notably, pregnancy during the first postpartum ovulation without prior menstruation is exceptionally rare and typically linked to abrupt reductions in breastfeeding intensity.
Many breastfeeding mothers report premenstrual symptoms, such as cramping, for weeks or months before menstruation resumes. These signs suggest hormonal adjustments toward fertility restoration, even as lactation delays its completion. The timeline for full fertility recovery varies widely, with earlier menstruation often correlating with a more gradual transition to full reproductive capacity.
This phased process underscores the complex interplay between lactation, hormonal regulation, and ovarian reactivation in postpartum physiology.
Breastfeeding and Conception: Navigating Fertility While Nursing
Is weaning necessary to achieve pregnancy?
Generally, weaning is not required to conceive. During the transition to full fertility—marked by gradual ovarian reactivation—breastfeeding may temporarily affect implantation success due to hormonal fluctuations. However, once implantation occurs, studies indicate breastfeeding does not compromise a healthy pregnancy, provided maternal nutritional needs are met. If menstrual cycles have resumed with regularity, lactation likely no longer suppresses fertility.
Many nursing mothers conceive without altering breastfeeding patterns, as individual hormonal responses vary widely. There is no universal threshold of nursing frequency or duration that guarantees conception. Some may benefit from gradually reducing feeds or shortening sessions, though toddlers often naturally decrease nursing as they age. Abrupt changes, such as eliminating nighttime feeds, often accelerate fertility restoration—even if breastfeeding continues extensively. This explains why fertility frequently returns when children sleep through the night or begin solid foods.
Research confirms that total daily nursing time and frequency—rather than specific timing of feeds—are the primary factors influencing fertility suppression. For instance, reducing a nighttime session versus a daytime one shows negligible difference in outcomes. While rare, a small subset of mothers may struggle to conceive while nursing, often linked to prolonged high-frequency breastfeeding patterns.
Regarding pregnancy testing, breastfeeding does not interfere with results. Tests detect human chorionic gonadotropin (hCG), a hormone produced after implantation, unaffected by lactation. Reliable detection typically occurs 7–14 days post-implantation.
In summary, most nursing mothers can conceive without weaning, though individualized adjustments to feeding patterns may optimize outcomes. Monitoring menstrual regularity and consulting healthcare providers for personalized guidance remain critical steps.