Milk production typically begins midway through pregnancy. For most mothers, a noticeable increase in milk volume—transitioning from colostrum to mature milk—occurs between days 2 and 5 after delivery.
Is there milk present at birth?
Yes! Colostrum, a nutrient-rich and antibody-packed early milk, starts forming as early as 16–22 weeks of pregnancy. Many mothers may not realize its presence initially, as it often doesn’t leak and can be challenging to express manually. This “liquid gold” is tailored to meet newborns’ needs during their first days of life, providing essential nutrients and immune protection.
At birth, a baby’s stomach is tiny (about the size of a marble), and the small volumes of colostrum (2–10 mL per feeding in the first 24 hours) are perfectly suited to their capacity. By day 3, intake typically rises to 30–60 mL (1–2 oz) per feeding as milk production transitions toward mature breast milk. Colostrum’s composition also aids in clearing meconium and reducing jaundice risks, further supporting early infant health.
This gradual shift aligns with hormonal changes post-birth, particularly the drop in progesterone and rise in prolactin, which trigger full lactation. Frequent breastfeeding or pumping during this period helps establish and maintain milk supply, ensuring the baby’s nutritional needs are met as their stomach grows.
Timing and Indicators of Postpartum Milk Supply Increase
Milk production typically initiates biochemical changes 30–40 hours after placental delivery. However, most mothers notice visible signs of increased supply—such as breast fullness, warmth, or swelling—around 2–3 days postpartum. For approximately 25% of mothers, this “milk coming in” phase may extend beyond three days.
Key indicators of increasing milk supply include:
- Physical breast changes: Heaviness, tingling, engorgement, or warmth.
- Leakage: Spontaneous milk flow, particularly during nighttime.
- Milk appearance: Gradual transition from golden, thick colostrum to thinner, whiter mature milk when expressing.
- Infant behavior: Altered feeding patterns, such as more frequent or vigorous nursing sessions.
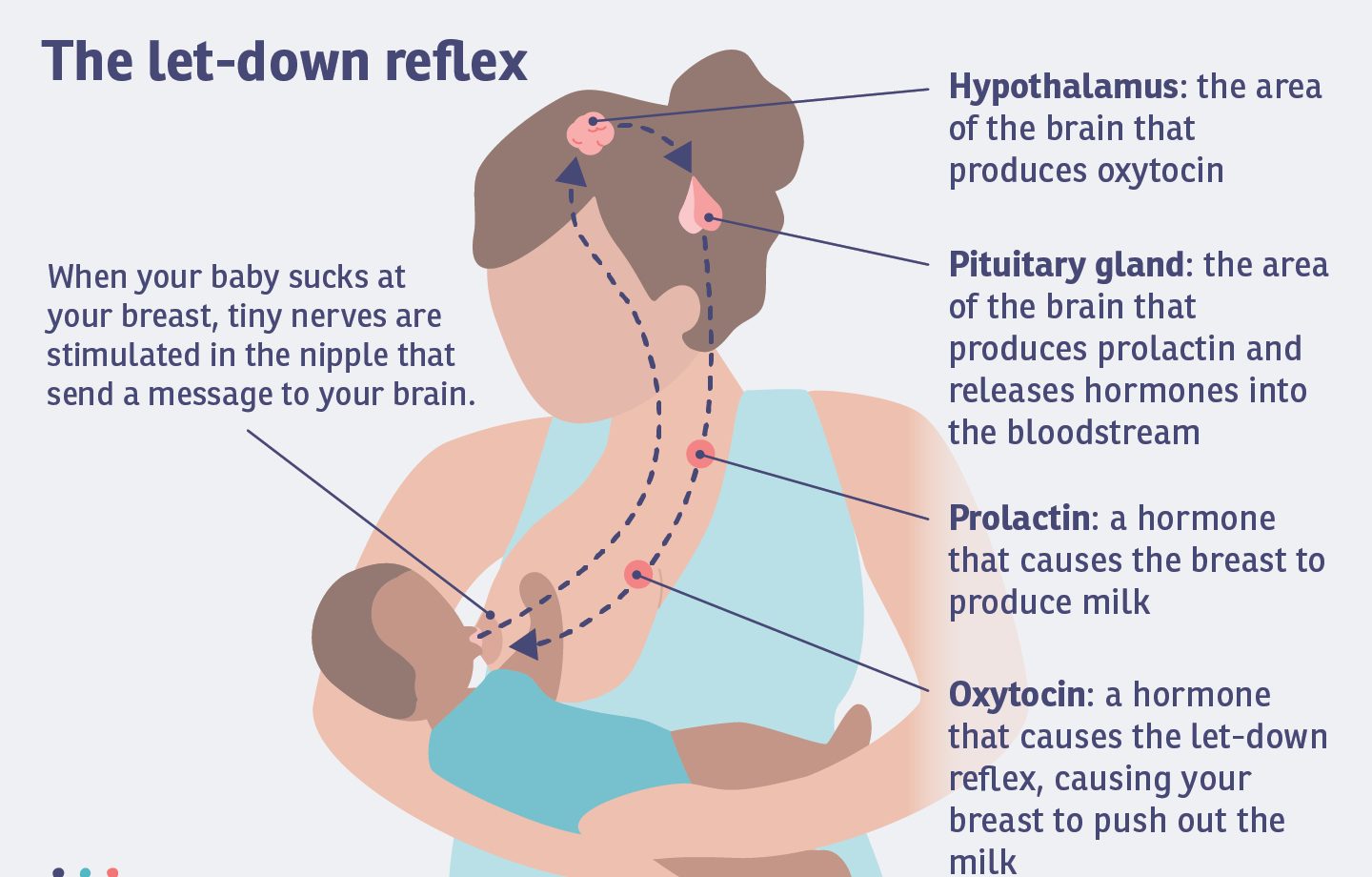
While hormonal shifts primarily regulate this process, proactive measures enhance outcomes. Frequent breastfeeding or pumping within the first 3–4 days correlates with higher milk volumes, reduced infant weight loss, and lower jaundice risk. Skin-to-skin contact further stimulates production by optimizing oxytocin release.
Notably, milk removal is critical during this phase. Without consistent nursing or expression, lactation may diminish even as supply begins to rise. Mothers should prioritize emptying breasts thoroughly through feeding or pumping to sustain and amplify production.
For those experiencing delays, patience is essential. Milk establishment often follows a gradual trajectory rather than an abrupt shift, with full maturation occurring around 10–15 days postpartum.
Delayed Onset of Lactation: Key Risk Factors and Underlying Causes
Delayed onset of lactation (DOL) refers to the failure of a mother’s milk supply to increase as expected within 72 hours postpartum. This delay can stem from diverse biological, hormonal, and management-related factors.
Maternal Characteristics
First-time mothers often experience later lactogenesis compared to multiparous individuals. Obesity and conditions affecting hormonal regulation—such as insulin resistance, poorly controlled type-1 diabetes, polycystic ovarian syndrome, hypothyroidism, or pituitary disorders like Sheehan’s syndrome—are strongly linked to DOL. Hypertension and gestational ovarian theca lutein cysts further elevate risks by disrupting endocrine pathways critical for milk production.
Labor and Delivery Complications
Prolonged labor stages, excessive blood loss (>500 mL), and cesarean sections (potentially due to surgical stress, medication effects, or delayed breastfeeding initiation) are significant contributors. Retained placental fragments may temporarily suppress lactation until resolved. High intravenous fluid administration during labor and analgesic use also correlate with delayed secretory activation.
Breast Anatomy and Management Challenges
Structural issues like mammary hypoplasia, prior breast surgery, or nipple abnormalities (e.g., inverted nipples) can impede milk transfer and removal. Preterm birth may limit prenatal glandular development, though proactive lactation support post-delivery can mitigate this. Medications such as hormonal contraceptives and inadequate early milk removal due to maternal illness or poor breastfeeding practices further exacerbate supply limitations.
Physiological Mechanisms
Emerging research suggests obesity-related DOL may involve altered prolactin responses or suboptimal breastfeeding management rather than true lactogenic failure. Stress and anxiety, prevalent in 17.4% of Chinese perinatal women, suppress oxytocin release and disrupt milk ejection reflexes.
Proactive interventions—including frequent nursing, skin-to-skin contact, and targeted support for high-risk groups—are critical to counteract these risks and promote timely lactogenesis.
Addressing Delayed Milk Production: Practical Guidance
If milk production has not begun by the fourth day postpartum, prioritize optimizing breastfeeding practices. Ensure frequent and thorough breast emptying through nursing or pumping, as consistent milk removal stimulates supply. Skin-to-skin contact with the infant can enhance oxytocin release, supporting both bonding and lactation.
Closely track the baby’s weight to assess intake. A weight loss exceeding 7% of birth weight necessitates immediate evaluation by a lactation specialist or pediatrician. If supplementation is required, use expressed breast milk, donor milk, or formula while continuing efforts to establish direct breastfeeding.
Consult a board-certified lactation consultant to develop a tailored plan. They may recommend techniques like power pumping, breast compression, or adjusting feeding positions to improve milk transfer. Medical evaluation is critical if underlying issues are suspected—retained placental fragments, hormonal imbalances (e.g., thyroid dysfunction, prolactin deficiency), or metabolic conditions like PCOS can delay lactation. Blood tests for thyroid hormones, prolactin, and testosterone may identify treatable causes.
For mothers recovering from a challenging start, persistence is key. Studies show that even with delayed onset, many achieve a full supply through consistent effort over weeks. Techniques such as herbal galactagogues (e.g., fenugreek, blessed thistle) or prescribed medications like domperidone may be considered under medical supervision.
Note: Stress and fatigue can further hinder production. Prioritize rest, hydration, and calorie-dense nutrition to support physiological recovery. Collaborate with healthcare providers to address both physical and emotional challenges during this transitional period.